One of the ideas which people perceive about Direct Primary Care is it’s only affordable for wealthier incomes. This article, which was well written by Marguerite Duane, MD, MHA, debunks the reasoning behind it. The link to the original article can be found at the bottom of the page.
So, if poor people have little to spend, why would the direct primary care model work for them? Simple; with direct pay models the actual health care costs can be kept much lower and therefore more affordable for these very patients. Plus, since direct pay models often have smaller patient panels, these patients may have more time with their physicians and staff to address the myriad of issues in their life that may be affecting their health.
Some direct pay models charge patients a monthly or yearly membership fee that covers all primary care office visits and even some basic or in-house labs. For example, at Qliance in Seattle, depending on the patients’ age, members pay a fee that ranges between $54 – $94 a month, which includes:
- 7 -day a week access to the Qliance health care team
- Same or next-day appointments for urgent care
- 30-60 minute office visits
- Phone appointments and e-visits
- After hour phone access to a physician for urgent medical needs
Sure, direct primary care is great because it covers all primary care visits, but you may wonder how will poor patients pay for labs or specialty visits? It may surprise you to learn that the actual cost of most basic labs is actually very little. We negotiated with local labs to pay just above the actual cost of the tests and in exchange, we pay our lab bill in full monthly. Here is an example of how it would work for a patient with diabetes:
Labs Actual Cost Patient Paid at time of visit
- HgAIC $8.72 $10
- Lipid panel $3.47 $ 5
- CMP $4.21 $ 5
What about the cost of specialty care, clearly this is much too expensive for poor people to afford, right? My response to that question is two-fold:
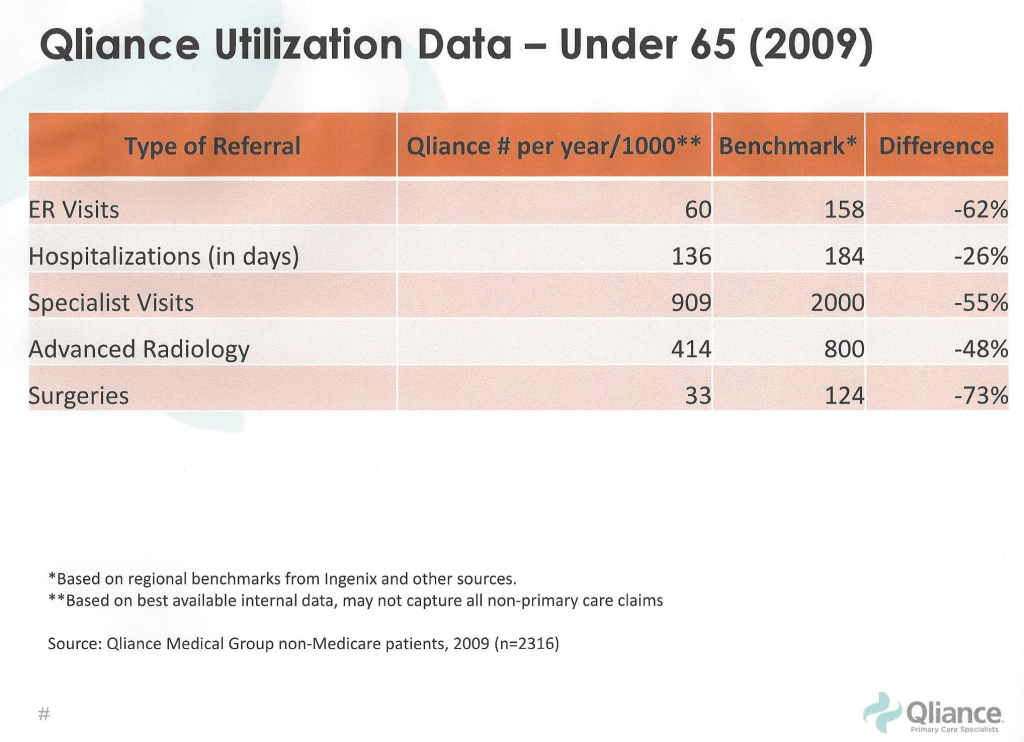
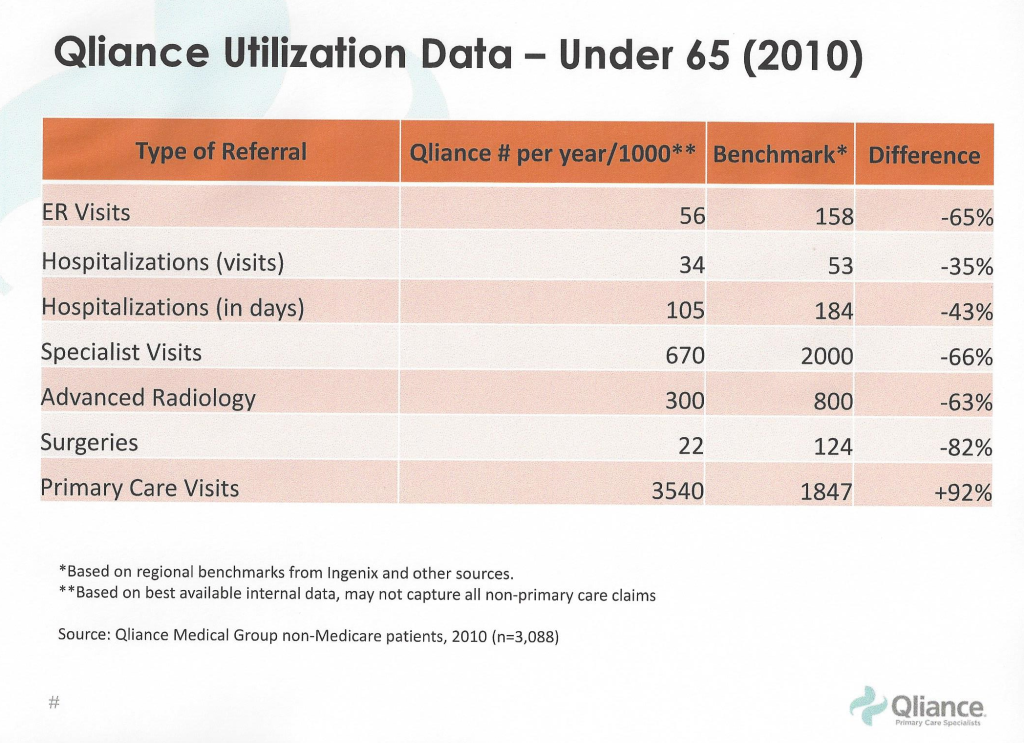
First, one of the main benefits of the direct primary care model is physicians have more time to spend with their patients to actually figure out what is wrong and treat problems appropriately; and therefore, they need to refer patients less often. As family physicians, I believe we are well trained to handle the myriad of problems that patients may present with, but we do not have enough time to adequately address them in a 10 minute office visit, so we often feel compelled to refer them to specialists. QIiance has demonstrated that when you have the time to spend with patient, specialist and ER visits, surgeries and hospitalizations are all significantly reduced
Second, even specialists are willing to reduce their fees when they are guaranteed payments in a more timely manner. Again, when we eliminate the insurance middleman, we significantly reduce the uncertainty and/or time it takes to pay for services. In reality, fees for sub-specialty visits, services, surgeries, etc. are set for insurance companies who routinely underpay by a significant amount, since they can negotiate much lower payments. Again, if we could eliminate the “insurance bureaucracy tax” by reducing administrative costs through the removal of the insurance middle man, specialists could charge patients much less for the actual services they provide.
The original article can be found here from The Direct Primary Care Journal

